Analyzing Digital Communities Used by Individuals Suffering with Chronic Pain
To showcase the important knowledge I have gained from the Culture & Technology Studies program at the University of Guelph, I produced a capstone project that aims to raise awareness of the lack of support doctors provide to patients with invisible and chronic pain.
Introduction
Individuals with autoimmune diseases, such as rheumatoid arthritis (RA) and ankylosing spondylitis (AS), experience many chronic symptoms that can affect their physical and mental well-being. Often described as an invisible illness, these symptoms and diagnoses cannot be seen by the naked eye but can limit an individual’s “movements [and] senses” (Salamon, 2023). Due to this, these individuals have unique experiences in and out of the medical sphere. I began exploring topics or concepts important to me for this project and landed on the experience of invisibility in the medical environment. As someone with chronic and autoimmune diseases, I had to advocate for myself in front of doctors for over five years to receive a diagnosis. Once I received this reassurance, the experiences I continued to have in my everyday life did not improve as I thought they would because others often overlook chronic pain due to its ‘invisible’ symptoms. Feeling like no one understands the physical and emotional pain that is felt throughout this experience often leaves individuals feeling lonely and hopeless. Most of this community finds support through Reddit to discuss their hardships, improvements, pain, and general support. Ultimately, I have received insight into how these digital communities are used and the kind of language featured in each.
To further understand the lack of support provided by healthcare practitioners, I focused my attention on four Reddit communities and their posted content. Specifically, r/ChronicIllness, r/Autoimmune, r/RheumatoidArthritis, and r/AnkylosingSpondylitis will be used to broaden my understanding of chronic pain while also looking into specific types of autoimmune diseases. It is important to note that RA and AS were chosen due to my previous knowledge and experiences with these conditions. RA is an “autoimmune and inflammatory disease” that primarily manifests in the individual’s joints, such as “hands, wrists, and knees,” as well as affects the body’s “lungs, heart, and eyes” (Rheumatoid Arthritis | CDC, 2022). AS is similar to RA, but in addition to the joints, it also targets an individual’s ligaments of the spine” in addition to the “knees, ankles, and hips” (Branch, 2023).
“I’ve had a heck of a start to the new year. I switched biologics in December due to some potential side effects […] and I went from doing absolutely amazing to absolutely terrible.
The switch caused a flare […] Then the flare caused my facet joints to act up again, and while I was previously stable from a prior RFA and the other biologic, the new med did not seem to quell the pain. […] Somewhere along the way, I managed to herniate four discs in both my neck and low back […] so now I’ve been having to do PT again.
But I have so many good things going on in my life as well, a positive career change that will allow me to educate and help others with autoimmune disease, a wonderful family with the most supportive husband I could ever ask for, an active social life. And yet…I’m finding that I’m totally blank. The things that should make me happy don’t and the things that should make me sad (like these health issues) I just feel like saying “whatever, what else is new”.
I don’t know if I’m just totally disassociating from feelings because of so many highs and lows recently or if I’ve just resigned myself to some sort of depression. I finally accepted that I may need some help with processing my feelings (like for instance the massive guilt I feel for having this disease and how at times it takes away from me being a good wife/mother) that I keep pushing down and ignoring. So I made an appointment for next week with a therapist I used to see years ago who I really trust as she was great for the issue I saw her for. Logically I know I’m doing the right thing, but the other part of me just feels like “Great, another doctor/appt”. “
– This disease takes such a mental toll.
Review of Relevant Scholarship
Increased Depression & Anxiety
Considering the unique and often dismissive experiences of those with autoimmune, invisible, or chronic illnesses, individuals have a much higher rate of depression and anxiety as compared to other communities (Euesden et al., 2017). It is also important to note that in addition to the physical symptoms, “the functional, educational, financial, occupational, and social impacts [experienced by these individuals] have been chronically overlooked due to rare disease invisibility” (Richards, 2022). Additionally, these communities often display “an impairment of health-related quality of life and exhibit depression-like symptoms” (Pryce & Fontana, 2016). Due to this, many individuals do not notice or acknowledge the daily struggles that chronic pain sufferers experience, which explains the importance of support within this community.
Age also plays a factor, as Euesden et al. investigated data from 23 autoimmune diseases and compared timelines between when autoimmune and depression symptoms started to occur (Euesden et al., 2017). The hypothesis was justified, as there was “significant comorbidity between depression and the autoimmune disorders,” more substantially ‘depression increased [the] subsequent hazard if autoimmune disorder onset […] independently of autoimmune disorder genetic risk” (Euesden et al., 2017). Through this study, one can acknowledge that many risk factors contribute to the link between autoimmune diseases and depression. Euesden et al. (2017) suggest these factors include “both common environmental exposures that increase baseline inflammation levels, and shared genetic factors” (Euesden et al., 2017). Understanding the correlation between chronic illnesses and depression is a crucial aspect of comprehending the kind of support that these individuals require to live long and happy lives.

As stated by researchers Christopher Pryce and Adriano Fontana, “The immune system not only leads to inflammation in affected organs, but also mediates behavior abnormalities including fatigue and depression-like symptoms” (Pryce & Fontana, 2016). Similarly, Endres et al. concluded that the subgroup of patients studied for their research experienced depressive symptoms directly caused by autoimmune diseases, such as multiple sclerosis and systemic lupus erythematosus (Endres et al., 2020). The term “autoimmune depression” is also mentioned in particular patients who experienced depressive symptoms for many years before any recent autoimmune diagnosis (Endres et al., 2020).
Complex Procedures.
Due to complex diagnosis procedures, patients often have to go through lengthy processes or trial and error to receive an accurate diagnosis, if any diagnosis at all. As Iglesias et al. (2018) state, “ Chronicity, and particularly complex care needs for people with chronic diseases, is one of the main challenges of health systems” (Iglesias et al., 2018). For example, there is no simple test to diagnose AS as an individual illness. Still, a blood test verifying the presence of the HLA-B27 gene can ultimately lead to a diagnosis when accompanied by various symptoms (Branch, 2023). It is a lengthy procedure to receive this diagnosis due to its complexity and knowledge of the disease, as “A lack of knowledge leads to difficulty in obtaining a diagnosis” (Richards, 2022. Due to this, chronic symptoms such as loss of appetite, abdominal pain, fatigue, and vision changes are often dismissed as they do not lead to a direct diagnosis (Branch, 2023). Additionally, due to the fact that chronic symptoms cannot be captured on physical tests, such as blood testing, it can be very difficult to narrow down the symptoms, leaving the patient undiagnosed. This may explain why many individuals have trouble obtaining a diagnosis and, therefore, seek support from those who have similar experiences. As a result, these individuals can often feel ignored or dismissed by their doctors and lonely when dealing with their symptoms.
Invisibility.
Among the many physical symptoms that accompany chronic illnesses, “educational, financial, occupational, and social impacts [are] chronically overlooked due to rare disease invisibility” (Richards, 2022). Due to the lack of research surrounding this concept, it is difficult to display the inequalities people living with chronic pain experience to the general public. Understanding the functional and social impacts of a global issue is crucial to ensure that the message and experiences of this community translate to those who cannot comprehend living with chronic pain. More notably, if these needs cannot be understood, “acquiring access to appropriate healthcare and social services, political commitment to addressing the inequalities, and incentivising research” is nearly impossible (Richards, 2022). Without the knowledge and preexisting research data, those in positions of power are uninformed of the needs of these individuals, further promoting a “selfperperuating invisibility cycle” (Richards, 2022).
Mental Health and Support
Support groups and other forms of community, such as self-organized forums, have been shown to increase individuals’ quality of life when dealing with chronic health conditions (Armstrong & Powell, 2009). Studies by Bingham et al. (2020) and Mossberger and Tolbert (2021) have focused on virtual discussion forums’ influence on an individual’s mental health and the reliability of the information posted to these communities. As can be applied to each area of an individual’s life, talking through one’s feelings and discussing hardships can improve their mental health (Bingham et al., 2020). It is crucial to understand that those who experience chronic pain and autoimmune disease symptoms tend to have a higher rate of depression and anxiety as “Autoimmune disease increases vulnerability to depression and other mental health challenges in general for biological, psychological, and social reasons” (Bingham et al., 2020). When turning to digital communities for support, healthcare practitioners have been advised to avoid this space due to the misleading medical advice that is often shared. Digital communities and support groups hold mighty power in the lives of those who use them; “Health practitioners should note that such communities can have clear empowering benefits and at the same time that concerns about the propagation of inaccurate or misleading information” (Armstrong & Powell, 2009).
Additionally, Sudau et al. (2014) reported that although users shared advice with other contributors, their sources were mainly opinions and personal experiences. Similarly, research conducted by Armstrong et al. (2009) using online diabetes communities concluded that virtual forum users greatly influence their readers’ opinions and medical outlook. Commonly, the results in each of their research stresses the concerns of misleading information being shared within the community. However, gaps in this research include individuals seeking emotional support, which is often overlooked. I will address this group in my research to understand how they use the digital community.
Addressing Concerns
This project aims to address the concerns of invisibility and lack of support provided to patients with chronic pain and autoimmune symptoms from healthcare practitioners. This was done by analyzing 2000 posts from digital communities outlining their various experiences. By looking at these online forums, I understood how these spaces were being used, which would later help me understand what kind of support is needed in the healthcare system. Additionally, my project highlights the dismissive behaviour often exhibited by healthcare practitioners and aims to shed light on the invisibility experienced by these individuals. This is evident in the final result of my project, as the majority of the top words used were ‘negative,’ and many of the posts were searching for some type of support or advice.
Each of my Anaconda workbooks containing my Python code can be found on my GitHub: https://github.com/japassare/r-SeekingSupport
Contextualization of Project & Social Implications
Addressing Concerns
This project aims to address the concerns of invisibility and lack of support provided to patients with chronic pain and autoimmune symptoms from healthcare practitioners. This was done by analyzing 2000 posts from digital communities outlining their various experiences. By looking at these online forums, I understood how these spaces were being used, which would later help me understand what kind of support is needed in the healthcare system. Additionally, my project highlights the dismissive behaviour often exhibited by healthcare practitioners and aims to shed light on the invisibility experienced by these individuals. This is evident in the final result of my project, as the majority of the top words used were ‘negative,’ and many of the posts were searching for some type of support or advice.
Methodology and Adaptation
For the central part of my project, I used Python to input, organize, and analyze my data directly from Reddit. I began by creating an API that would pull my desired number of posts from each subreddit and store them on Python. These were organized and included the post title, body, link, and number of likes and comments. Next, I removed any necessary stop words from my text, such as ‘that,’ ‘it,’ and ‘is,’ to clean up my data and only have significant words be included for my next step of sentiment analysis. Finding a library that would help me run sentiment analysis proved to be a challenge. I tried several sentiment libraries initially, but the output was not as straightforward or structured as I would have liked, so I switched to VADER. Using VADER, I ran sentiment analysis through my code to produce a numeral score of whether the individual post was negative, neutral, or positive. This went very smoothly, and I could produce a .csv file with all the necessary information and the sentiment score to analyze later.
After reviewing the results of each post, I quickly realized that I disagreed with the sentiment scores and decided to look deeper to understand what was going wrong. My code worked perfectly, but most posts received either a neutral score or a slightly positive score, which is not what I had initially hypothesized. I could simply read through the posts to understand that the sentiment scores did not reflect the actual sentiment of the posts.
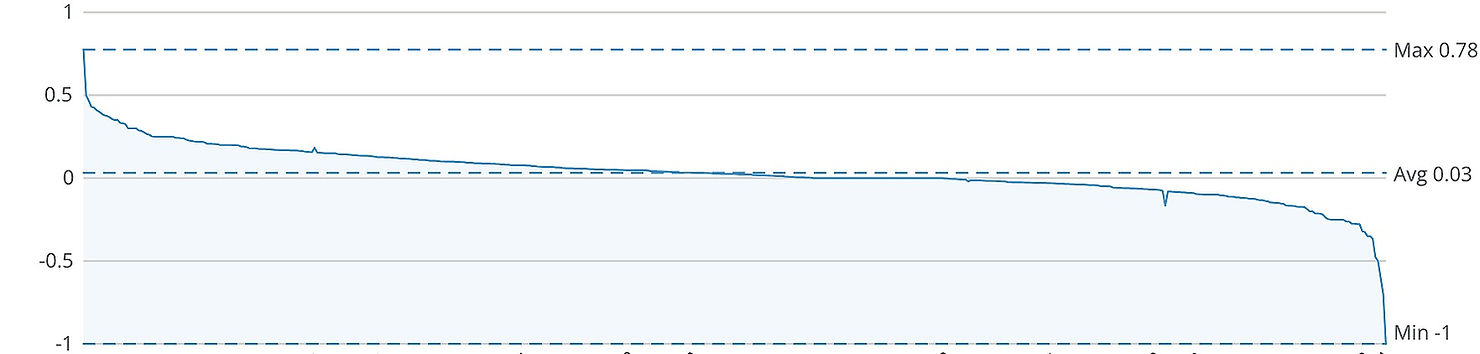
To prove this, I did the whole process again, but this time with the individual words as opposed to the whole post. First, I used Python to calculate the frequency of the words, and then I ran my sentiment analysis through the list of individual words. Similar to my previous sentiment analysis, a large portion of my data received a neutral score. For example, the second most used word, ‘back,’ had a neutral (0) sentiment score, most likely because the word ‘back’ is often used like the term ‘previously’ or ‘before.’ At this point, I started to understand why so many words were not receiving an accurate score. I have the background knowledge that RA and AS often target an individual’s spine and can lead to a high level of back pain. In this case, not only can I assume, but I can contextualize that the second most used word, ‘back,’ refers to the physical back and spine. This would lead me to score the word as negative because it is being used as a way to describe the location of pain. This was when my project switched from just using a computational tool to analyze text to comparing computerized and interpretive methods.
Missing Pieces
Although my project does a good job highlighting the lack of support that achronic pain and autoimmune disease patients receive, there are some areas of research that are not fully accounted for. For instance, individuals tend to act differently online as opposed to in person. Perhaps taking this into account would have swayed the final outcome of my research, but for the purpose of my project, I decided to take the posts as they were. Additionally, understanding the location of those postings would have been an essential factor to consider. Healthcare drastically differs from country to country, so it would have been very interesting to see where the posts were coming from to understand the context around their experiences. Similarly, cold and wet weather can often worsen chronic symptoms; therefore, it would have been crucial to note if a post was made from a colder climate.
Social Implications
Through this work, I hope the results and data can be shared online to show the importance of care and support. I believe that the social implications of my project manifest in the increase of education and equality, specifically in the medical sphere. If healthcare practitioners are not educated on the specific support required for individuals suffering from chronic and autoimmune diseases, they are unable to provide adequate care to the patient. Through my work, I hope this research will improve this community’s overall mental well-being and help them get the support they require. Ultimately, this project promotes equality and aims to improve those within these communities’ medical and social experiences.
Resources
Armstrong, N., & Powell, J. (2009). Patient perspectives on health advice posted on Internet discussion boards: a qualitative study. Health Expectations, 12(3), 313–320. https://doi.org/10.1111/j.1369-7625.2009.00543.x
Bingham, K., Rozenbojm, N., Chong-East, M., & Touma, Z. (2020). Exploring the mental health needs of persons with autoimmune diseases during the Coronavirus Disease 2019 pandemic: A Proposed Framework for future research and Clinical care. ACR Open Rheumatology, 3(1), 25–33. https://doi.org/10.1002/acr2.11205
Branch, N. S. C. a. O. (2023, December 15). Ankylosing spondylitis. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/ankylosing-spondylitis
Endres, D., Rauer, S., Venhoff, N., Süß, P., Dersch, R., Runge, K., Fiebich, B. L., Nickel, K., Matysik, M., Maier, S., Domschke, K., Egger, K., Prüß, H., & Van Elst, L. T. (2020). Probable autoimmune depression in a patient with multiple sclerosis and antineuronal antibodies. Frontiers in Psychiatry, 11. https://doi.org/10.3389/fpsyt.2020.00745
Euesden, J., Danese, A., Lewis, C. M., & Maughan, B. (2017). A bidirectional relationship between depression and the autoimmune disorders – New perspectives from the National Child Development Study. PloS One, 12(3), e0173015. https://doi.org/10.1371/journal.pone.0173015
Iglesias, F. H., Celada, C. A., Navarro, C. B., Morales, L. P., Visus, N. A., Valverde, C. C., Dorado, V. M., Muñoz, M. L. M., Blay, C., Ramírez, E. L., Villaroel, R. M., Jordana, N. M., & Bonet-Simó, J. M. (2018). Complex care needs in multiple chronic conditions: population prevalence and characterization in primary care. a study protocol. International Journal of Integrated Care, 18(2). https://doi.org/10.5334/ijic.3292
Mossberger, K., & Tolbert, C. J. (2021). Digital citizenship and digital communities. International Journal of E-planning Research, 10(3), 19–34. https://doi.org/10.4018/ijepr.20210701.oa2
Pryce, C. R., & Fontana, A. (2016). Depression in autoimmune diseases. In Current topics in behavioral neurosciences (pp. 139–154). https://doi.org/10.1007/7854_2016_7
Rheumatoid arthritis | CDC. (2022, April 7). Centers for Disease Control and Prevention. https://www.cdc.gov/arthritis/types/rheumatoid-arthritis.html#:~:text=Rheumatoid%20arthritis%2C%20or%20RA%2C%20is,usually%20many%20joints%20at%20once.
Richards, D. (2022). Seeing Is Believing: Invisibility Exacerbates Inequality for Patients Living with Rare Disease. European Medical Journal. https://doi.org/10.33590/emj/10149519
Salamon, M. (2023, May 1). Invisible illness: More than meets the eye. Harvard Health. https://www.health.harvard.edu/diseases-and-conditions/invisible-illness-more-than-meets-the-eye
Sudau, F., Friede, T., Grabowski, J., Koschack, J., Makedonski, P., & Himmel, W. (2014). Sources of information and behavioral patterns in online health forums: Qualitative study. JMIR. Journal of Medical Internet Research/Journal of Medical Internet Research, 16(1), e10. https://doi.org/10.2196/jmir.2875
Acknowledgements
r/AnkylosingSpondylitis. (n.d.). Reddit. https://www.reddit.com/r/ankylosingspondylitis/
r/Autoimmune. (n.d.). Reddit. https://www.reddit.com/r/Autoimmune/
r/ChronicIllness. (n.d.). Reddit. https://www.reddit.com/r/ChronicIllness/
Grammarly.
Procreate.
r/RheumatoidArthritis. (n.d.). Reddit. https://www.reddit.com/r/rheumatoidarthritis/
Leave a comment